Über mich
In the hectic world of medical care, administrative tasks like prior authorization can decrease individual care and bewilder facility staff. Understanding and handling the procedure successfully is crucial for getting therapies approved and compensated. In this overview, we'll discover what prior authorization is, why it matters, just how it functions, and how facilities can improve the procedure to lower hold-ups and enhance individual outcomes.
What Is Previous Consent?
Prior permission (PA), also understood as pre-authorization or pre-certification, is a demand from medical insurance companies that specific solutions, medications, or treatments have to be accepted before they are provided to the patient. It acts as a cost-control process, ensuring that the asked for service is medically essential and covered under the patient's insurance coverage plan.
Why Is Prior Authorization Essential for Centers?
Avoid Denials and Unpaid Claims
Without prior permission, insurance provider might refute coverage, leaving clients and clinics liable for the cost.
Make Sure Appropriate Care
It works as a check to avoid unneeded or duplicative therapies, lining up with evidence-based standards.
Maintain Compliance
Meeting insurance coverage requirements assists prevent lawful issues and sustains smooth profits cycle administration.
When Is Previous Permission Called For?
Every insurance carrier has its own checklist of solutions needing authorization, but common instances consist of:
Advanced imaging (e.g., MRI, CT checks).
Specialized drugs.
Elective surgical treatments.
Durable clinical equipment (DME).
Non-emergency hospital admissions.
Psychological wellness services.
Centers need to examine each client's prepare for details requirements.
The Previous Authorization Refine: Step-by-Step.
Determine the Requirement.
Validate if the asked for service or drug needs prior authorization.
Send the Demand.
Gather and send out the necessary clinical records, carrier notes, diagnostic outcomes, and forms to the insurance policy carrier.
Wait on Testimonial.
The insurer examines the documents. This can take anywhere from a few hours to numerous days.
Obtain the Choice.
The demand is either approved, rejected, or returned for added info.
Communicate with the Person.
Notify the patient of the result and next steps. If refuted, the facility may assist appeal the choice.
Difficulties Facilities Confront With Previous Consents.
Taxing Refine: Team may invest hours handling phone telephone calls, faxes, and documentation.
Delays in Patient Care: Waiting on approval can hold off essential treatments.
Rejections and Appeals: Insufficient or wrong submissions can cause denials.
Absence of Standardization: Various insurers have different policies, making it challenging to develop one system for all.
Exactly how to Enhance the Refine in Your Center.
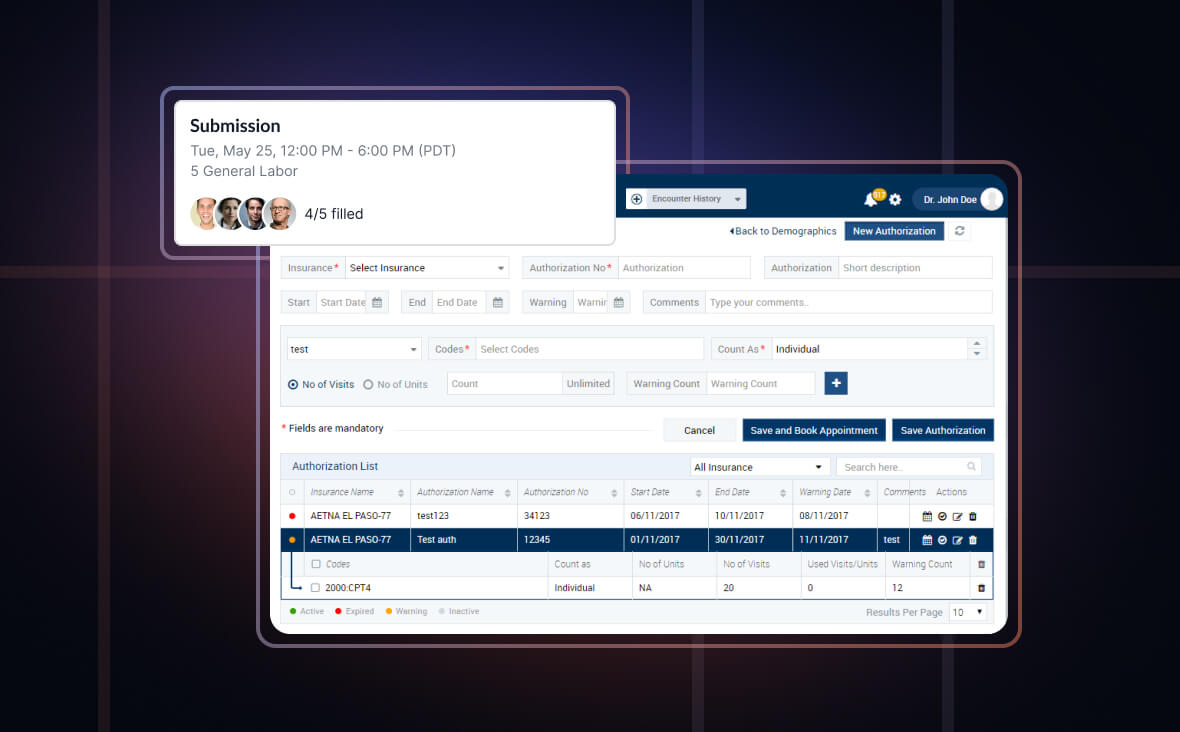
✅ Use Previous Permission Software Program.
Automation devices and EHR-integrated systems can decrease manual labor and track status updates in real-time.
✅ Train and Delegate.
Train dedicated personnel or hire a prior consent specialist or virtual assistant to take care of submissions, follow-ups, and allures efficiently.
✅ Develop a List.
Preserve a reference sheet for each and every insurance policy company's PA needs for your center's most typical solutions.
✅ Remain Proactive.
Confirm insurance policy qualification and demands throughout person intake or prior to scheduling solutions.
✅ Track Outcomes and Metrics.
Screen approval prices, turn-around times, and common denials to boost procedures and minimize errors.
Partnering with a Prior Consent Virtual Assistant.
One economical remedy is to contract out prior consent jobs to a digital medical aide. These specialists:.
Take care of entry and follow-up.
Reduce administrative problem on in-clinic team.
Help prevent pricey hold-ups and rejections.
Are trained in collaborating with different EHR and insurance policy systems.
By handing over these tasks, clinics can concentrate much more on client treatment and much less on documents.
Conclusion.
Prior permission is a necessary but usually discouraging component of modern-day health care. By recognizing the process and carrying out wise options-- like automation tools or online aides-- clinics can decrease management burdens, improve individual satisfaction, and safe much faster approvals. With the ideal systems in position, your center can turn prior permission from a bottleneck right into a structured part of your client treatment operations.
In the hectic world of healthcare, administrative jobs like prior consent can reduce down individual treatment and overwhelm facility personnel. In this guide, we'll explore what prior permission is, why it matters, just how it functions, and exactly how centers can simplify the process to reduce delays and enhance client outcomes.
Prior consent is an essential yet commonly discouraging part of modern-day medical care. By comprehending the procedure and carrying out clever options-- like automation tools or online assistants-- clinics can lower management burdens, enhance client satisfaction, and safe faster approvals. With the appropriate systems in place, your clinic can transform prior consent from a traffic jam right into a streamlined part of your client treatment process.
Ort
Beruf

